Hypervigilance: Signs, Causes & How to Calm Your Overactive Nervous System
Author: Dr. Timothy Rubin, PhD in Psychology
Originally Published: December 2025
Last Updated: December 2025
Hypervigilance keeps your nervous system on high alert even when you're safe, making it difficult to relax and feel at peace.
Contents
- What Is Hypervigilance?
- The Science: A Nervous System Stuck in Fight-or-Flight
- Hypervigilance vs. General Anxiety
- How to Calm Hypervigilance: 3 Evidence-Based Strategies
- How AI Tools Can Help Regulate Your Nervous System
- Frequently Asked Questions
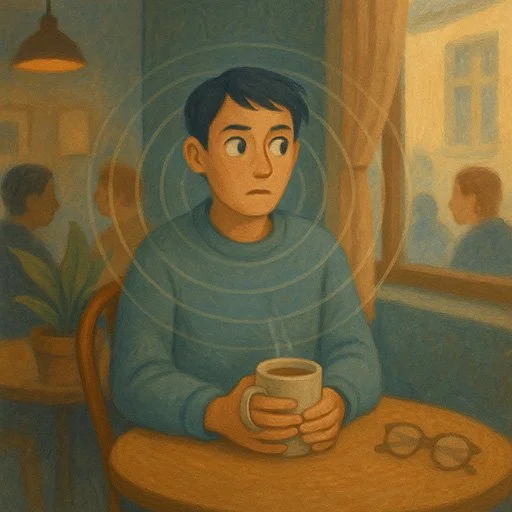
Have you ever felt like you can't fully relax, even when you know you're safe? Maybe you startle easily, constantly scan rooms for potential threats, or find it impossible to "turn off" that feeling of needing to be on guard. You might be experiencing hypervigilance—a state where your nervous system gets stuck in "fight or flight" mode, convinced danger lurks around every corner.
Hypervigilance is more than ordinary anxiety. It's an exhausting, constant state of high alert that can significantly impact your quality of life. The good news? With understanding and the right techniques, you can retrain your nervous system to feel safe again. Let's break down what hypervigilance is, what causes it, and—most importantly—how you can start calming it today.
What Is Hypervigilance?
Hypervigilance is a survival mechanism that becomes overactive, keeping you constantly scanning for threats that aren't there.
Hypervigilance is a state of elevated sensory sensitivity and heightened awareness, where your brain is constantly on the lookout for danger—even when none is present. It's like your internal alarm system never turns off. Ordinary events—a door slamming, someone walking behind you—might trigger an intense reaction. You're ready to spring into action at any moment.
While a healthy level of vigilance keeps us safe (like looking both ways before crossing a street), hypervigilance goes overboard. People experiencing hypervigilance often:
- Feel constantly "on edge" and unable to fully relax
- Startle easily at sudden noises or movements
- Scan their environment continuously, checking for potential threats
- Experience muscle tension from being perpetually "ready to react"
- Have difficulty sleeping because their mind/body won't "shut down"
- Misinterpret neutral or harmless cues as dangerous
Hypervigilance is commonly associated with Post-Traumatic Stress Disorder (PTSD), where the nervous system learned from past trauma that the world is a dangerous place. However, it can also appear in other anxiety conditions, after periods of intense stress, or in situations where someone's safety was threatened for an extended period.
The Science: A Nervous System Stuck in Fight-or-Flight
When the amygdala stays activated, your body remains in a constant state of fight-or-flight readiness.
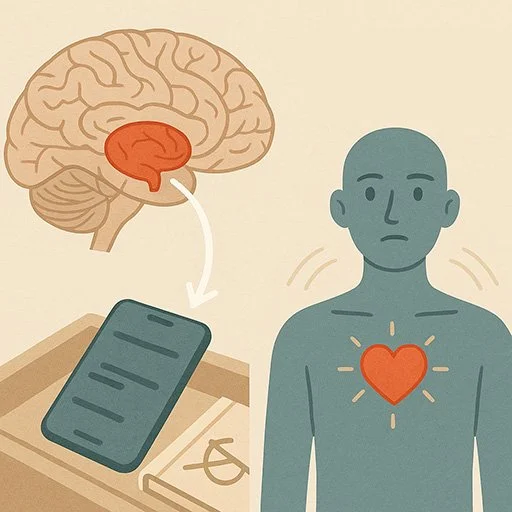
To understand hypervigilance, it helps to know how your nervous system responds to threat. When you perceive danger, your amygdala (the brain's alarm center) activates your body's fight-or-flight response. Stress hormones like cortisol and adrenaline flood your system, your heart rate increases, muscles tense, and attention narrows to focus on the threat.
This response is supposed to be temporary—it saves your life when facing a real threat (like a car speeding toward you). After the danger passes, your parasympathetic nervous system should activate the "rest and digest" mode, calming everything down. Your body relaxes, heart rate slows, and you return to baseline.
However, after trauma or prolonged stress, that alarm system can get "stuck." Your amygdala becomes overactive, perceiving threats where there are none. It's as if your nervous system is constantly shouting, "Danger! Stay alert!" even when you're sitting safely on your couch. This chronic activation exhausts your body and mind.
Neurologically, this involves altered threat perception circuits in your brain. The amygdala's fear response overpowers the prefrontal cortex (which normally helps you rationally assess danger). Essentially, the emotional, reactive part of your brain is in the driver's seat, leaving the calm, rational part in the back. This is why logical reassurances like "You're safe" often don't help much—your body believes otherwise.
Hypervigilance vs. General Anxiety
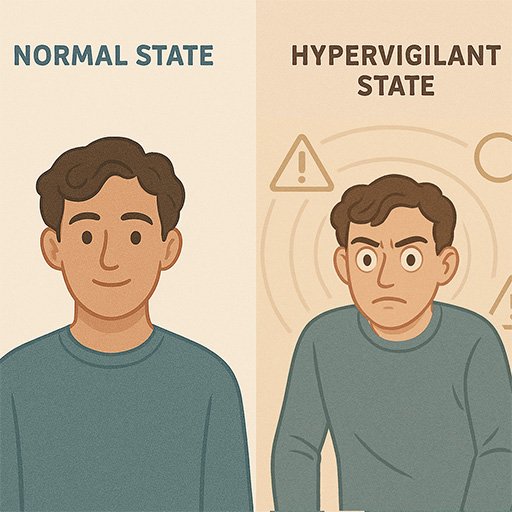
You might be wondering: Isn't hypervigilance just anxiety? They're related, but not the same.
General anxiety involves excessive worry about various things—health, work, relationships, the future. You might feel nervous about an upcoming presentation or worry about whether you locked the door. It's often more cognitive (thought-based).
Hypervigilance, on the other hand, is more sensory and immediate. It's a heightened state of scanning your current environment for threats right now. You're not just worried about a vague future—you're convinced danger is imminent at this moment. Your senses are amplified. A creak in the house becomes a burglar; a stranger on the street feels menacing.
While generalized anxiety can involve some hypervigilance, hypervigilance is often more extreme and tied to trauma. It's a hallmark symptom of PTSD that distinguishes it from other anxiety disorders. If you have PTSD, you might constantly feel like you're back in a dangerous situation, even years later.
How to Calm Hypervigilance: 3 Evidence-Based Strategies
Learning to calm your nervous system is essential for overcoming hypervigilance and reclaiming a sense of safety.
The key to managing hypervigilance is retraining your nervous system to recognize safety. This doesn't happen overnight, but with practice, you can signal to your body that it's okay to relax. Here are three evidence-based strategies that target hypervigilance at its root:
1. Grounding Techniques: Return to the Present Moment
Hypervigilance pulls you into a threat-focused state where past trauma feels current. Grounding techniques help anchor you in the here-and-now, reminding your nervous system that you're safe right now.
The 5-4-3-2-1 Technique: A popular grounding method. Slowly name:
- 5 things you can see (a picture on the wall, your phone, a plant…)
- 4 things you can touch (the texture of your shirt, the chair beneath you…)
- 3 things you can hear (distant traffic, a clock ticking, your breathing…)
- 2 things you can smell (coffee, soap, fresh air…)
- 1 thing you can taste (a sip of water, residual toothpaste…)
This exercise forces your brain to engage with your current environment using your senses, pulling you out of threat mode. As you focus on benign details, you're subtly communicating to your amygdala: "I'm safe. Nothing dangerous is happening right now."
Orienting: Another powerful grounding method. Slowly look around the room without moving your head too much. As you notice objects, mentally note: "I see a lamp. I see a window. I see a bookshelf." This helps your nervous system map the actual environment—not the imagined threats. After a minute or two, remind yourself out loud: "I'm in my living room. It's [current date and time]. I'm safe."
For more grounding exercises, see our article on grounding techniques for panic attacks.
2. Nervous System Regulation: Breathing & Body-Based Techniques
Since hypervigilance is rooted in an overactive sympathetic nervous system (fight-or-flight), you need to activate its counterpart: the parasympathetic nervous system (rest-and-digest). Certain techniques physiologically calm your body down.
Extended Exhale Breathing: This is one of the fastest ways to signal safety to your nervous system. When you exhale longer than you inhale, you stimulate the vagus nerve, which activates the parasympathetic system.
Try this: Inhale through your nose for 4 counts, then exhale slowly through your mouth for 6-8 counts. Repeat for several minutes. The long exhale tells your body: "No emergency here—we can slow down." Over time, your heart rate decreases, muscles relax, and the hypervigilant state softens.
Bilateral Stimulation (Butterfly Hug): This technique is used in trauma therapies like EMDR (Eye Movement Desensitization and Reprocessing). Cross your arms over your chest and gently tap your shoulders alternately—left, right, left, right—at a steady, slow rhythm. This bilateral stimulation (activating both sides of the body/brain) can help process trauma and reduce hyperarousal.
It might sound simple, but research suggests bilateral stimulation helps integrate traumatic memories and calm the nervous system. Try it for 1-2 minutes whenever you notice hypervigilance creeping in.
Cold Water Splash: Splashing your face with cold water or holding ice cubes can activate the dive reflex, instantly slowing your heart rate and calming panic. This is a quick "reset button" for your nervous system when hypervigilance spikes.
3. Gradual Exposure & Reprocessing Trauma
Hypervigilance is often rooted in unprocessed trauma. Your brain and body are still reacting as if the traumatic event is happening. To truly resolve hypervigilance (not just manage it), you may need to process the underlying trauma.
Exposure Therapy: Gradually and safely confronting trauma-related memories or situations can help your brain learn that these triggers are no longer dangerous. For example, if you're hypervigilant in crowded places due to past trauma, you might slowly expose yourself to busier environments while using grounding and breathing techniques. Over time, your brain updates its threat assessment: "Crowded places aren't inherently dangerous."
This should ideally be done with a trained therapist, especially if the trauma was severe. EMDR and trauma-focused Cognitive Behavioral Therapy (CBT) are two evidence-based methods that help reprocess traumatic memories so they no longer trigger hypervigilance.
Somatic Therapy: Since trauma lives in the body as much as the mind, somatic approaches focus on releasing stored tension and teaching the body to feel safe again. Techniques might include gentle movement, breathwork, or body awareness exercises.
How AI Tools Can Help Regulate Your Nervous System

AI-powered mental health tools provide personalized, on-demand support for managing hypervigilance and calming your nervous system.
Managing hypervigilance requires consistent practice, which is where technology can help. While nothing replaces professional therapy for severe trauma, AI-powered mental health tools like Wellness AI can provide valuable, personalized support between therapy sessions—or as a first step if you're not ready for formal treatment.
Personalized, On-Demand Meditation
One challenge with traditional meditation apps is that they offer generic recordings. If you're hypervigilant, though, your nervous system has specific triggers and needs. AI-generated meditations can be tailored to your unique situation.
For instance, Wellness AI creates custom guided meditations based on what you're experiencing right now. If you tell the app you're feeling hypervigilant after a stressful meeting, it can generate a meditation that specifically targets nervous system regulation—perhaps incorporating grounding imagery, extended exhales, and gentle reminders of safety. This level of personalization helps your brain receive exactly the message it needs to calm down.
The app's meditation generation considers your history, so over time, it learns what techniques work best for you (progressive muscle relaxation? Visualization? Breathwork?). This adaptive approach can be more effective than one-size-fits-all recordings. Learn more about body scan meditation techniques that can help with hypervigilance.
24/7 Support for Processing Anxious Thoughts
Beyond meditation, an AI companion like Wellness AI's chat can help you process anxious thoughts and provide cognitive techniques in the moment. When you're feeling hypervigilant, sometimes talking (or typing) through what you're experiencing can bring relief and perspective. The AI therapist is available 24/7, meaning you have someone to talk to in those high-anxiety moments at 2 AM.
Importantly, the AI learns about you over time—it remembers your triggers, your values, and what coping strategies work for you. This allows it to offer more personalized support with continued use. Many people find this kind of consistent, on-demand support helps reinforce what they might also be learning in therapy by giving them daily practice.
Building Routine and Tracking Progress
Tools like Wellness AI can also help you track your progress and maintain routines that impact your nervous system, such as sleep, exercise, and regular meditation practice. The app might remind you to practice a nighttime meditation for better sleep, or celebrate with you when you take one of those micro-actions we discussed. This positive reinforcement and tracking can motivate you to keep using the techniques that calm your hypervigilance.
What makes AI particularly promising is personalization and immediacy. Traditional resources like generic meditation recordings are one-size-fits-all. In contrast, an AI wellness app can tailor its responses and exercises to you in real time. If you're experiencing a spike of hypervigilance after a stressful meeting, you could pull out the app, describe what you're feeling, and it might generate a calming strategy on the spot.
Of course, AI is not a replacement for professional therapy, especially for deep-seated trauma. But it is a valuable complement. By providing consistent, personalized support and relaxation practices, an app like Wellness AI can help retrain your nervous system over time. For more information on how AI therapy can support mental health, check out our article on the latest research on AI therapy effectiveness.
When to Seek Professional Help
While self-help techniques can be effective, it's important to seek professional help if hypervigilance is severely impacting your life, if you're experiencing suicidal thoughts, or if you have a history of significant trauma. Trauma-informed therapists trained in modalities like Cognitive Behavioral Therapy (CBT), EMDR, or somatic therapy can provide specialized support for healing hypervigilance at its roots.
Related Resources
For more information on related topics, explore these guides:
Remember: if you're struggling with hypervigilance, you're not "crazy" or alone—your brain is doing what it thinks it must to protect you. With understanding, practice, and support, you can teach it that it's safe to relax again. Take it one day at a time, celebrate small victories, and don't hesitate to seek professional help if needed. You deserve to live with a sense of calm and safety.
-Tim, Founder of Wellness AI
About the Author
Dr. Timothy Rubin holds a PhD in Psychology with a focus on cognitive science and the application of AI in mental health treatment. His research has been published in peer-reviewed psychology and artificial intelligence journals. Dr. Rubin is particularly interested in trauma-informed approaches and the neuroscience of emotional regulation. He founded Wellness AI to make evidence-based mental health support more accessible through technology.
Frequently Asked Questions
What are the signs of hypervigilance?
Key signs include feeling constantly on guard and unable to relax, an exaggerated startle response (jumping at sudden noises or movements), and continually scanning your environment for threats. Hypervigilant people often experience muscle tension, trouble sleeping, and a tendency to interpret ordinary things as potential dangers. If you always feel tense and ready to spring into action as if something bad is about to happen, those are telltale signs.
How is hypervigilance different from general anxiety?
Hypervigilance is anxiety on overdrive with a focus on immediate threats. While general anxiety involves excessive worry about various things (money, health, future events), hypervigilance means you feel unsafe right now and are constantly scanning your environment every second, even when you're objectively safe. It's a core feature of PTSD that distinguishes it from ordinary anxiety disorders.
What causes hypervigilance?
The most common cause is trauma. If you've been through a traumatic or life-threatening event, your brain might stay in survival mode as a protective mechanism—leading to hypervigilance. Combat veterans, abuse survivors, or people who lived through disasters often report being hypervigilant. Chronic high stress, certain anxiety disorders, and even some medical conditions (like hyperthyroidism) can also trigger hypervigilant states.
Can hypervigilance be cured or go away?
With the right strategies and time, hypervigilance can significantly improve. Many people who practice consistent trauma-informed therapy or self-help techniques are able to reduce their hypervigilant responses and feel safe again in their daily lives. Treatments like cognitive-behavioral therapy, EMDR, and nervous system regulation practices have strong track records. It's absolutely possible to go from constant hypervigilance to only occasional moments of it, or none at all.
What can I do in the moment to calm hypervigilance?
Try deep breathing with longer exhales (inhale for 4 counts, exhale for 6-8 counts), orienting exercises where you look around and name things you see while reminding yourself "I'm safe right now," the butterfly hug with alternating tapping, or splashing cold water on your face. These immediate tools help signal safety to your nervous system and can quickly reduce the intensity of fight-or-flight responses. After you've calmed a bit, follow up with a relaxing activity like a short meditation or gentle stretches.