CBT vs. DBT for Anxiety: Understanding the Differences and When to Use Each
Author: Dr. Timothy Rubin, PhD in Psychology
Originally Published: May 2025
Last Updated: June 2025
CBT and DBT are both evidence-based therapies that take different approaches to treating anxiety and emotional challenges.
Contents
- What Is CBT (Cognitive Behavioral Therapy)?
- What Is DBT (Dialectical Behavior Therapy)?
- Key Differences Between CBT and DBT
- CBT vs. DBT for Anxiety—Which Is Better?
- Making the Choice: Which Therapy Should You Try?
- Digital Tools for CBT and DBT Practice
- Getting Started with Therapy
- FAQ: CBT vs DBT
Cognitive behavioral therapy techniques and dialectical behavior therapy skills are two popular talk therapies you might have heard about—especially if you're dealing with anxiety, depression, or intense emotions. They sound similar (both even have Behavioral Therapy in their names) and do share some roots, but they have key differences in focus and technique.
If you're wondering about the differences between CBT vs DBT for anxiety, or which might be a better fit for your needs, this therapy comparison guide breaks down what each therapy involves and who benefits most from each approach.
Both CBT and DBT are evidence-based therapy approaches—large bodies of research show both improve mental health and reduce anxiety symptoms. They simply take different paths to get there. Think of CBT vs DBT therapy as two tools in a toolbox: each tool is suited to certain jobs.
What Is CBT (Cognitive Behavioral Therapy)?

CBT focuses on the interconnected relationship between thoughts, feelings, and behaviors to create positive change.
Cognitive behavioral therapy techniques focus on the link between your thoughts, feelings, and behaviors. By reshaping unhelpful thought patterns and behaviors, you can change how you feel. Therapists help you spot cognitive distortions ("I'm going to fail at everything"), challenge them, and replace them with realistic thoughts while practicing new behaviors such as gradual exposure to fears.
Dozens of meta-analyses confirm CBT's effectiveness for anxiety and depression in clinical settings.
How CBT Works for Anxiety Treatment
CBT anxiety treatment options are typically structured and goal-oriented—often 8-20 sessions—and include homework like thought records or relaxation practice. Because it delivers practical skills quickly, CBT is considered a first-line therapy for anxiety disorders and mild-to-moderate depression.
Core CBT Techniques
- Cognitive restructuring - Identifying and challenging negative thought patterns
- Behavioral activation - Increasing engagement in positive activities
- Exposure therapy - Gradual confrontation of feared situations
- Problem-solving skills - Systematic approaches to life challenges
- Relaxation techniques - Managing physical anxiety symptoms
What Is DBT (Dialectical Behavior Therapy)?
DBT combines acceptance strategies with change techniques, helping people manage intense emotions effectively.
DBT for anxiety and depression is a specialized offshoot of CBT created by psychologist Marsha Linehan for treating borderline personality disorder (BPD). The term dialectical reflects its balance of two opposites: acceptance and change. DBT helps people accept intense emotions as valid in the moment while working to change the behaviors that accompany those emotions.
The Four DBT Skill Modules
Dialectical behavior therapy skills programs usually mix weekly individual therapy with group skills training in:
- Mindfulness—present-moment awareness borrowed partly from meditation techniques
- Distress tolerance—crisis-survival tools (e.g., paced breathing, holding ice) to endure intense pain without making things worse
- Emotion regulation—strategies to manage and shift powerful feelings over time
- Interpersonal effectiveness—skills to assert needs, set boundaries, and handle conflict
Research on DBT Effectiveness
Research shows DBT reduces self-harm and suicidal behavior in high-risk clients and has been successfully adapted for PTSD, eating disorders, substance misuse, adolescent behavioral problems, and chronic depression. Many therapists now use DBT skills training even for clients without BPD who struggle with emotional intensity and interpersonal difficulties.
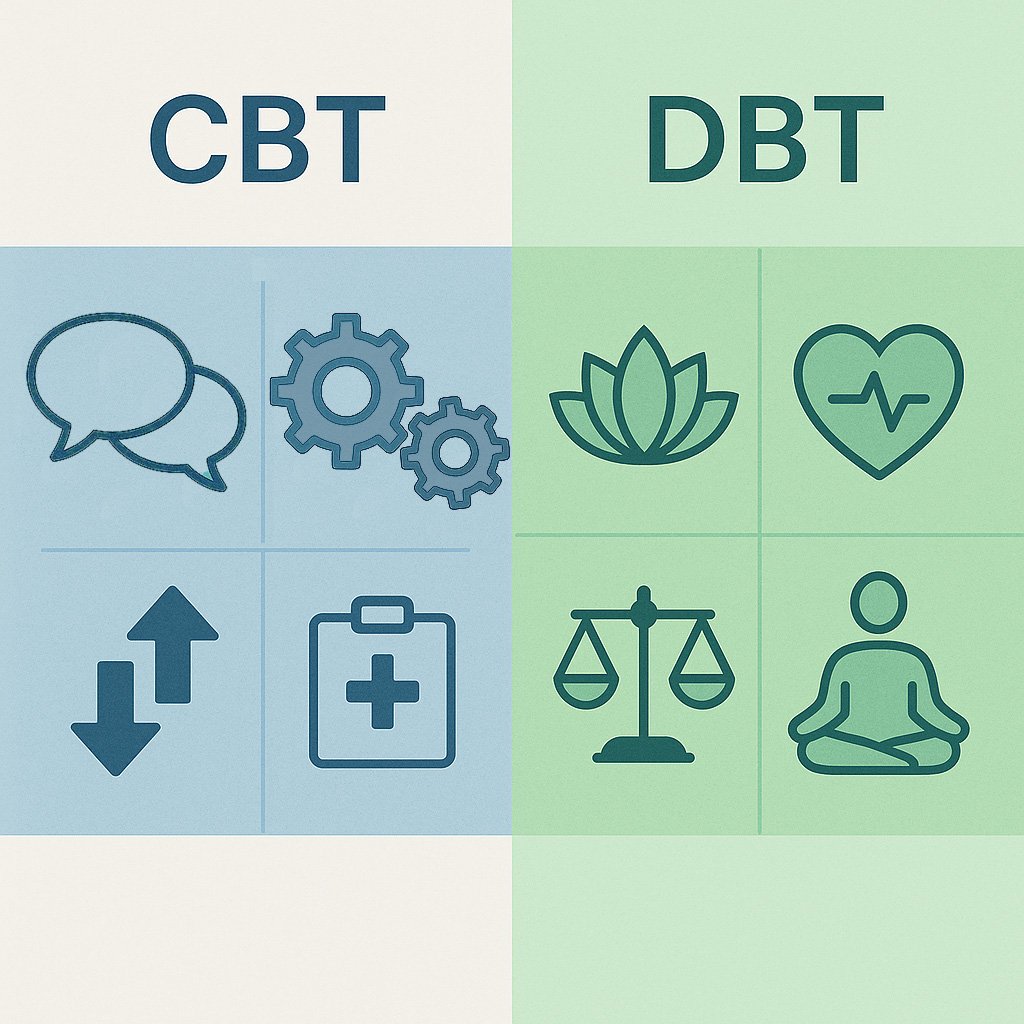
Key Differences Between CBT and DBT
Primary Focus Differences
CBT vs DBT therapy approaches differ in their primary focus: CBT targets distorted thoughts and avoidance behaviors; DBT pairs change work with radical self-acceptance (think "fix the problem" vs. "accept yourself and work on the problem").
Skills and Techniques
Cognitive behavioral therapy techniques emphasize cognitive restructuring, problem-solving, and graded exposure. Dialectical behavior therapy skills add mindfulness, distress tolerance, and emotion-regulation drills backed by studies linking improved skills to symptom gains.
Target Populations
CBT's evidence spans anxiety, depression, PTSD, insomnia, and OCD. While DBT was originally designed for BPD, it's now widely used for anyone struggling with emotional intensity, including those with chronic depression, eating disorders, addiction, trauma responses, and adolescent behavioral challenges. Meta-analyses show significant reductions in suicidal behaviors and improved emotional regulation across diverse populations.
CBT vs. DBT for Anxiety—Which Is Better?
Choosing between CBT and DBT for anxiety depends on your specific symptoms and emotional regulation needs.
CBT for Classic Anxiety Disorders
For most classic anxiety disorders (GAD, panic, social anxiety, phobias), CBT anxiety treatment options are usually the first choice because they directly tackle catastrophic thinking and avoidance behaviors as recommended by NIMH guidelines. A CBT plan might teach you to challenge "What if I embarrass myself?" thoughts and gradually face feared situations until anxiety shrinks.
When DBT Helps with Anxiety
DBT for anxiety and depression isn't typically the primary treatment for standard anxiety, but its mindfulness and distress-tolerance skills can be powerful add-ons—helping clients ride out panic peaks or overwhelming worry. Therapists often blend DBT tools into CBT when intense emotions derail exposure work.
Anxiety with Co-occurring Conditions
When depression co-occurs with anxiety, CBT still excels at shifting negative thought patterns, but DBT's focus on building a "life worth living" can help clients who feel chronically empty or impulsive. Clinical reviews note DBT's effectiveness for mood instability in difficult-to-treat populations.
Making the Choice: Which Therapy Should You Try?
Choose CBT If:
- Your main issues are anxious thoughts, phobias, or mild-to-moderate depression
- You prefer structured, goal-oriented therapy approaches
- You want to focus on changing thought patterns and behaviors
- You're looking for shorter-term therapy (8-20 sessions typically)
Consider DBT If:
- You struggle with overpowering emotions or emotional instability
- You have a history of self-harm or suicidal thoughts
- Relationships feel consistently unstable or conflicted
- You need better crisis-survival and distress-tolerance skills
- You experience emotional intensity that interferes with daily life
- Traditional CBT hasn't been fully effective for your needs
Either way, you'll gain active, skills-based strategies with strong research backing. Both therapies aim to empower you—CBT by changing how you think, DBT by changing how you handle intense feelings—so you can move forward with less anxiety and greater resilience.
Integrated Approaches in Real-World Practice
It's worth noting that many experienced therapists don't strictly adhere to one approach. In real-world clinical practice, therapists often integrate cognitive behavioral therapy techniques with dialectical behavior therapy skills based on what each client needs. For example, a therapist might use CBT's cognitive restructuring for anxious thoughts while incorporating DBT's distress tolerance skills for managing overwhelming emotions. This flexible, personalized approach often yields the best results.
Digital Tools for CBT and DBT Practice

Digital therapy tools can supplement traditional CBT and DBT with convenient skill practice and ongoing support.
Modern technology has made both cognitive behavioral therapy techniques and dialectical behavior therapy skills more accessible through digital platforms. These tools can supplement traditional therapy or provide standalone support for those who cannot access in-person treatment.
Benefits of Digital Therapy Support
- 24/7 availability when anxiety or emotional crises strike
- Consistent skill practice between therapy sessions
- Privacy and accessibility for those hesitant about traditional therapy
- Personalized approaches that adapt to your specific needs
For example, Wellness AI can provide personalized therapy conversations that incorporate CBT techniques like cognitive restructuring and behavioral activation, while also offering guided meditations that complement both CBT and DBT approaches to emotional regulation.
Getting Started with Therapy
Whether you choose CBT vs DBT therapy, the most important step is beginning the process. Both approaches require active participation and practice to be effective. Start by:
- Consulting with a mental health professional to assess your specific needs
- Researching therapists who specialize in your chosen approach
- Setting realistic expectations about the therapy process
- Committing to practicing skills outside of sessions
Remember that evidence-based therapy approaches like CBT and DBT have helped millions of people manage anxiety, depression, and emotional challenges. With the right fit and consistent effort, you can develop the skills to live a more balanced, fulfilling life.
-Tim, Founder of Wellness AI
About the Author
Dr. Timothy Rubin holds a PhD in Psychology with expertise in cognitive science and AI applications in mental health. His research has been published in peer-reviewed psychology and artificial intelligence journals. Dr. Rubin founded Wellness AI to make evidence-based mental health support more accessible through technology.
FAQ: CBT vs DBT
What is the main difference between CBT and DBT?
The main difference is focus: CBT primarily targets changing negative thought patterns and behaviors, while DBT balances acceptance of intense emotions with skills to change problematic behaviors. CBT asks "How can I think differently?" while DBT asks "How can I accept this feeling and respond wisely?"
Can you do both CBT and DBT at the same time?
Yes, and this is quite common in practice. Many therapists routinely integrate techniques from both approaches rather than strictly following one model. You might work on cognitive restructuring (CBT) for anxious thoughts while also learning mindfulness and distress tolerance skills (DBT) for emotional overwhelm. This integrative approach is often more effective than using either therapy in isolation, as it addresses both thinking patterns and emotional regulation.
Which therapy is better for anxiety disorders?
CBT is typically the first-line treatment for most anxiety disorders (GAD, panic disorder, social anxiety, phobias) because it directly addresses anxious thoughts and avoidance behaviors. However, DBT can be helpful when anxiety is accompanied by intense emotions, self-harm behaviors, or relationship difficulties.
How long does each therapy typically take?
CBT is typically shorter-term, lasting 8-20 sessions over 3-6 months. DBT is usually longer-term, often involving 6-12 months of weekly individual therapy plus group skills training. The duration depends on your specific needs and goals.
Is one therapy more effective than the other?
Both therapies are highly effective, but for different issues. CBT has the strongest evidence base for anxiety disorders and depression. DBT is most effective for emotion dysregulation, borderline personality disorder, and self-harm behaviors. The "better" therapy depends entirely on your specific symptoms and needs.
Do I need a diagnosis to benefit from CBT or DBT?
No formal diagnosis is required to benefit from either therapy approach. Both CBT and DBT teach valuable life skills that can help anyone manage stress, relationships, and emotional challenges more effectively. Many people use these techniques for personal growth and improved mental wellness.